Inilah pilihan tepat bagi Anda yang gemar bermain togel online! Dalam artikel ini, kami akan membahas keluaran togel terlengkap dan tercepat untuk memenuhi kebutuhan Anda dalam bermain judi togel. Tidak hanya itu, kami juga akan memberikan informasi mengenai keluaran togel Hongkong, Singapore, dan Sydney, sehingga Anda dapat selalu update dengan hasil-hasil terbaru.
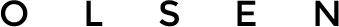
Setiap hari, Anda dapat menemukan informasi tentang hasil pengundian togel dari berbagai pasaran seperti Hongkong (HK), Singapore (SGP), dan Sydney (SDY) secara akurat dan terpercaya. Data keluaran ini dapat membantu Anda dalam merencanakan strategi bermain agar dapat memperoleh peluang menang yang lebih tinggi. Dengan demikian, Anda tidak perlu khawatir lagi tentang keakuratan data keluaran, karena kami menyediakan informasi yang terpercaya dan terupdate.
Selain itu, kami juga menyediakan data lengkap mengenai pengeluaran togel dari berbagai pasaran. Data ini meliputi keluaran Hongkong, Singapore, dan Sydney dalam satu tempat, sehingga memudahkan Anda dalam mencari dan membandingkan angka-angka yang keluar pada pasaran tersebut. Dengan data yang lengkap dan terpercaya, Anda dapat memanfaatkannya untuk meningkatkan peluang kemenangan Anda dalam bermain togel online.
Dalam dunia togel online, kecepatan adalah kunci. Oleh karena itu, kami menyediakan keluaran togel dengan cepat dan tepat waktu. Dapatkan hasil-hasil keluaran togel terbaru hanya dalam hitungan menit setelah pengundian selesai dilakukan. Dengan kecepatan ini, Anda dapat langsung merencanakan strategi bermain Anda dan memberikan kesempatan terbaik dalam meraih kemenangan.
Tidak hanya itu, kami juga memberikan informasi tentang data togel sgp hk sdy, togel hk sdy sgp, togel hk sgp sdy, togel sgp sdy hk, togel sdy hk sgp, dan togel sdy sgp hk. Informasi ini dapat membantu Anda dalam melacak angka-angka yang sering keluar atau berbagai pola terkait hasil keluaran togel dari pasaran-pasaran tersebut.
Tanpa perlu repot-repot mencari informasi keluaran togel secara manual, Anda dapat mengandalkan kami sebagai sumber informasi yang terpercaya dan terlengkap. Dapatkan keluaran togel tercepat dan terupdate hanya dengan mengunjungi situs kami. Togel online tidak pernah semudah ini sebelumnya! Selamat bermain dan semoga sukses dalam meraih kemenangan!
Keunggulan Togel Online Terlengkap dan Tercepat
Togel online merupakan sebuah platform yang menyediakan berbagai keunggulan dan kemudahan bagi para penggemar togel. Dalam artikel ini, kita akan membahas keunggulan-keunggulan yang membuat togel online terlengkap dan tercepat di antara opsi lainnya.
Pertama, keunggulan utama yang ditawarkan oleh togel online adalah keluaran terlengkap. Dengan akses ke berbagai pasaran togel seperti Hongkong, Singapore, dan Sydney, pemain dapat memilih dari berbagai pilihan yang tersedia. Ini membuka peluang lebih besar untuk memenangkan hadiah besar.
Selain keluaran terlengkap, togel online juga menawarkan keluaran togel tercepat. Dengan update yang dilakukan secara real-time, pemain dapat dengan cepat mengetahui hasil dari nomor togel yang mereka pasang. Ini memberikan keuntungan bagi pemain yang ingin segera mengetahui apakah mereka memenangkan taruhan atau tidak.
Selanjutnya, pengeluaran togel yang cepat juga menjadi salah satu keunggulan togel online. Dengan proses pembayaran yang mudah dan cepat, pemain dapat dengan cepat mencairkan hadiah yang mereka menangkan. Ini memberikan kenyamanan dan kepuasan bagi para pemain.
Dengan data togel yang selalu diperbarui, pemain juga dapat memiliki akses ke data hk, data sgp, dan data sdy. Hal ini memungkinkan pemain untuk menganalisis statistik togel sebelum memasang taruhan mereka, meningkatkan peluang mereka untuk memenangkan hadiah.
Di atas adalah beberapa keunggulan togel online terlengkap dan tercepat. Dengan fitur-fitur ini, pemain dapat menikmati pengalaman bermain togel yang lebih menyenangkan dan menguntungkan. Togel online adalah pilihan tepat bagi para penggemar togel yang ingin merasakan kepraktisan dan kecepatan dalam bermain dan memenangkan taruhan togel.
Pilihan Keluaran Togel Hongkong, Singapore, dan Sydney
Ada begitu banyak situs togel online yang menyediakan pilihan keluaran yang lengkap dan tercepat untuk togel Hongkong, Singapore, dan Sydney. Tidak perlu lagi repot-repot mencari informasi keluaran di berbagai sumber, karena dengan situs togel online ini, Anda dapat menemukan semua data yang Anda butuhkan dalam satu tempat. keluaran sgp
Situs togel online ini menyediakan keluaran togel Hongkong, Singapore, dan Sydney secara terlengkap. Anda dapat melihat data keluaran dengan mudah dan cepat hanya dengan beberapa klik. Tidak hanya itu, situs ini juga menyediakan pengeluaran togel dari beberapa periode sebelumnya, sehingga Anda dapat melakukan analisis dan perhitungan berdasarkan data yang sudah ada.
Dengan pengeluaran togel yang terupdate secara real-time, Anda dapat memperoleh informasi secara akurat mengenai hasil keluaran togel Hongkong, Singapore, dan Sydney. Dalam situs tersebut, Anda juga dapat melihat data-data penting seperti statistik, grafik, dan tabel dari keluaran togel sebelumnya, yang dapat membantu Anda dalam membuat strategi dan prediksi.
Togel online menjadikan semua data keluaran togel Hongkong, Singapore, dan Sydney lebih mudah diakses dan dipahami. Dengan menggunakan situs togel online ini, Anda dapat menghemat waktu dan tenaga dalam mencari informasi terbaru mengenai keluaran togel. Selain itu, Anda juga dapat memanfaatkan fitur-fitur unggulan yang ada dalam situs tersebut, seperti pengeluaran togel dengan visualisasi yang menarik dan pengeluaran togel dengan pembaruan yang cepat.
Jadi, bagi Anda yang mencari pilihan keluaran togel Hongkong, Singapore, dan Sydney yang lengkap dan tercepat, tidak ada salahnya mencoba situs togel online ini. Dapatkan informasi keluaran togel Hongkong, Singapore, dan Sydney dengan mudah, akurat, dan cepat melalui situs togel online yang dapat Anda akses kapanpun dan dimanapun Anda mau.
Data Togel Terpercaya: HK, SGP, SDY
Di dunia perjudian togel online, keakuratan dan kecepatan pengeluaran data togel sangat penting. Bagi para penggemar togel, memiliki data togel terpercaya adalah kunci untuk merencanakan strategi permainan mereka. Dalam artikel ini, kami akan membahas data togel terpercaya dari tiga pasaran ternama: Hongkong (HK), Singapura (SGP), dan Sydney (SDY).
-
Data Togel Hongkong (HK)
Pasaran togel Hongkong (HK) sangat populer di kalangan pemain togel online. Dalam mencari data togel HK yang terpercaya, penting untuk memilih sumber yang dapat memberikan hasil keluaran yang akurat dan tercepat. Dengan memiliki data togel HK yang terpercaya, pemain dapat menganalisis pola keluaran angka dan mengoptimalkan strategi permainan mereka.
-
Data Togel Singapura (SGP)
Pasaran togel Singapura (SGP) juga sangat diminati oleh pemain togel online. Dalam mencari data togel SGP yang terpercaya, penting untuk memilih sumber yang dapat menjamin keandalan data keluaran. Dengan memiliki data togel SGP yang terpercaya, pemain dapat memprediksi angka yang mungkin keluar dan meningkatkan peluang kemenangan mereka.
-
Data Togel Sydney (SDY)
Pasaran togel Sydney (SDY) adalah salah satu pasaran favorit di dunia perjudian togel online. Mempunyai data togel SDY yang terpercaya adalah kunci untuk membantu pemain membuat keputusan dalam permainan mereka. Dengan data togel SDY yang akurat dan tercepat, pemain dapat meningkatkan kemampuan mereka dalam menganalisis angka yang keluar dan meningkatkan peluang untuk memenangkan hadiah.
Dalam merencanakan strategi permainan togel online, mempunyai data togel terpercaya dari pasaran Hongkong (HK), Singapura (SGP), dan Sydney (SDY) adalah hal yang sangat penting. Pemain dapat melihat pola keluaran angka dan membuat prediksi yang lebih akurat dengan bantuan data togel yang akurat dan terupdate. Ingatlah untuk selalu memilih sumber data togel yang terpercaya agar dapat meraih kemenangan dalam permainan togel online.